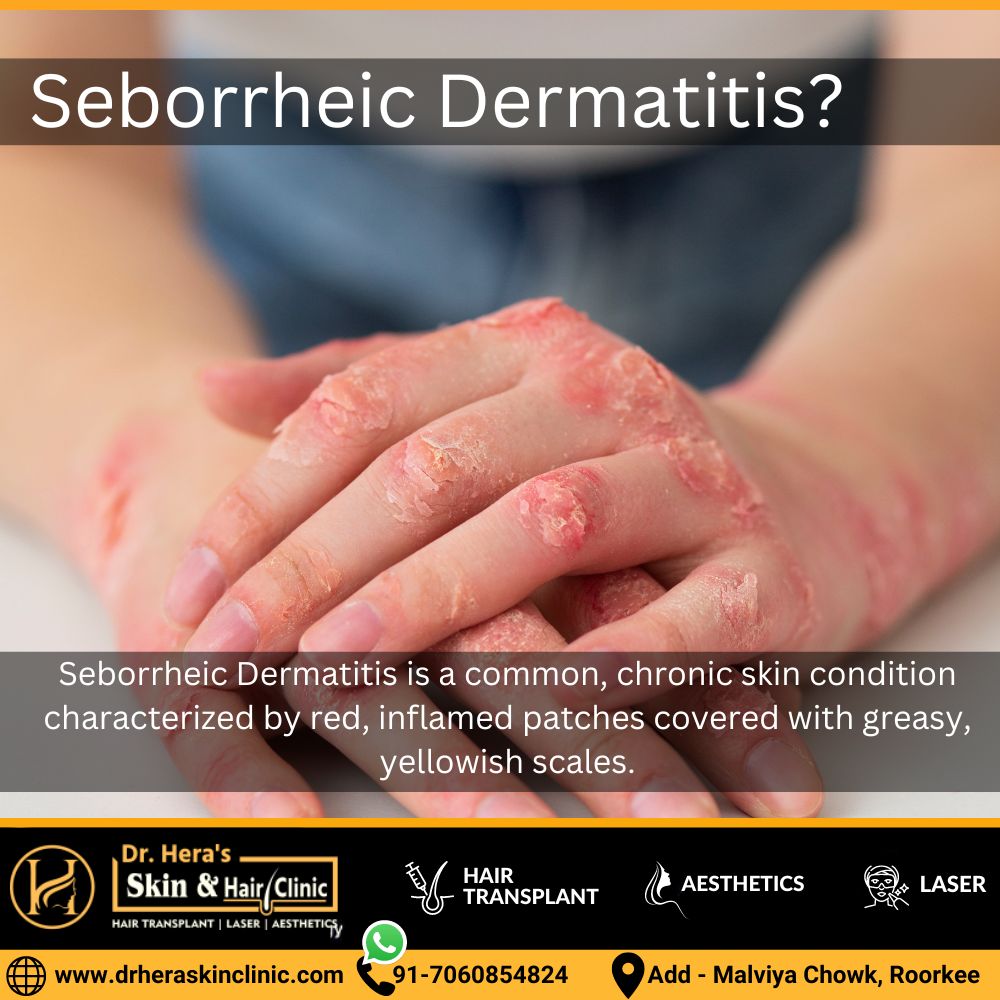
Know About Seborrheic Dermatitis
Seborrheic Dermatitis is a common, chronic skin condition characterized by red, inflamed patches covered with greasy, yellowish scales. It primarily affects areas rich in oil glands, such as the scalp, face, and chest. The exact cause is unclear, but factors like genetics, yeast overgrowth, and immune system responses contribute to its development. Symptoms often include itching, burning, and flaking skin.
While not curable, Seborrheic Dermatitis can be managed through various treatments, including medicated shampoos, topical steroids, antifungal agents, and lifestyle adjustments. Although the condition is generally benign, it can have a significant impact on quality of life, causing discomfort and self-consciousness. Maintaining good hygiene, avoiding triggers, and using prescribed medications are crucial for long-term management. Individuals experiencing persistent or severe symptoms should consult a dermatologist for a tailored treatment plan to alleviate symptoms and improve overall skin health.
Causes of seborrheic dermatitis
Seborrheic Dermatitis is a multifactorial skin condition, and its exact cause remains unclear. However, several factors are believed to contribute to its development:
- Yeast Overgrowth: The yeast Malassezia, which is normally present on the skin, can overgrow and trigger inflammation, leading to seborrheic dermatitis.
- Genetics: A family history of seborrheic dermatitis may increase the likelihood of developing the condition, suggesting a genetic predisposition.
- Hormonal Changes: Fluctuations in hormones, particularly during puberty, pregnancy, and certain medical conditions, can influence the development of seborrheic dermatitis.
- Stress: Emotional or physical stress is considered a potential trigger, exacerbating symptoms or contributing to the onset of the condition.
- Immune System Response: Abnormal immune responses may play a role, as the condition often manifests in areas rich in oil glands where the immune system is actively involved.
- Neurological Factors: Some researchers believe that neurological factors may contribute to the development of seborrheic dermatitis, although the mechanisms are not fully understood.
Understanding these potential causes can guide treatment strategies and lifestyle adjustments to manage seborrheic dermatitis effectively. Individuals experiencing persistent or severe symptoms should seek professional medical advice for a comprehensive evaluation and personalized treatment plan.
Treatment for seborrheic dermatitis
Treatment for seborrheic dermatitis often involves a comprehensive approach implemented by dermatologists to manage symptoms effectively. The specific treatment plan may vary based on the severity of the condition and individual factors. Common approaches include:
Topical Antifungal Medications:
Dermatologists may prescribe antifungal creams, ointments, or shampoos containing ingredients like ketoconazole, selenium sulfide, or ciclopirox to reduce the overgrowth of yeast on the skin.
Corticosteroids:
Topical corticosteroids can help alleviate inflammation and itching associated with seborrheic dermatitis. However, they are typically used for short periods to avoid side effects.
Calcineurin Inhibitors:
Topical calcineurin inhibitors, such as tacrolimus and pimecrolimus, may be recommended to control inflammation and reduce symptoms.
Medicated Shampoos:
Specialized shampoos with active ingredients like ketoconazole, coal tar, or salicylic acid can effectively manage seborrheic dermatitis on the scalp.
Prescription-strength Treatments:
In cases of severe or persistent seborrheic dermatitis, dermatologists may prescribe stronger medications, such as oral antifungal agents or oral corticosteroids.
Lifestyle Recommendations:
Dermatologists may provide guidance on proper skincare routines, including gentle cleansing and moisturizing. Avoiding triggers, such as certain skincare products or dietary factors, may also be advised.
Regular follow-ups with the dermatologist in Roorkee are essential to monitor progress and make adjustments to the treatment plan as needed. Individuals should consult a dermatologist for a personalized evaluation and tailored treatment approach based on their unique condition and medical history.
