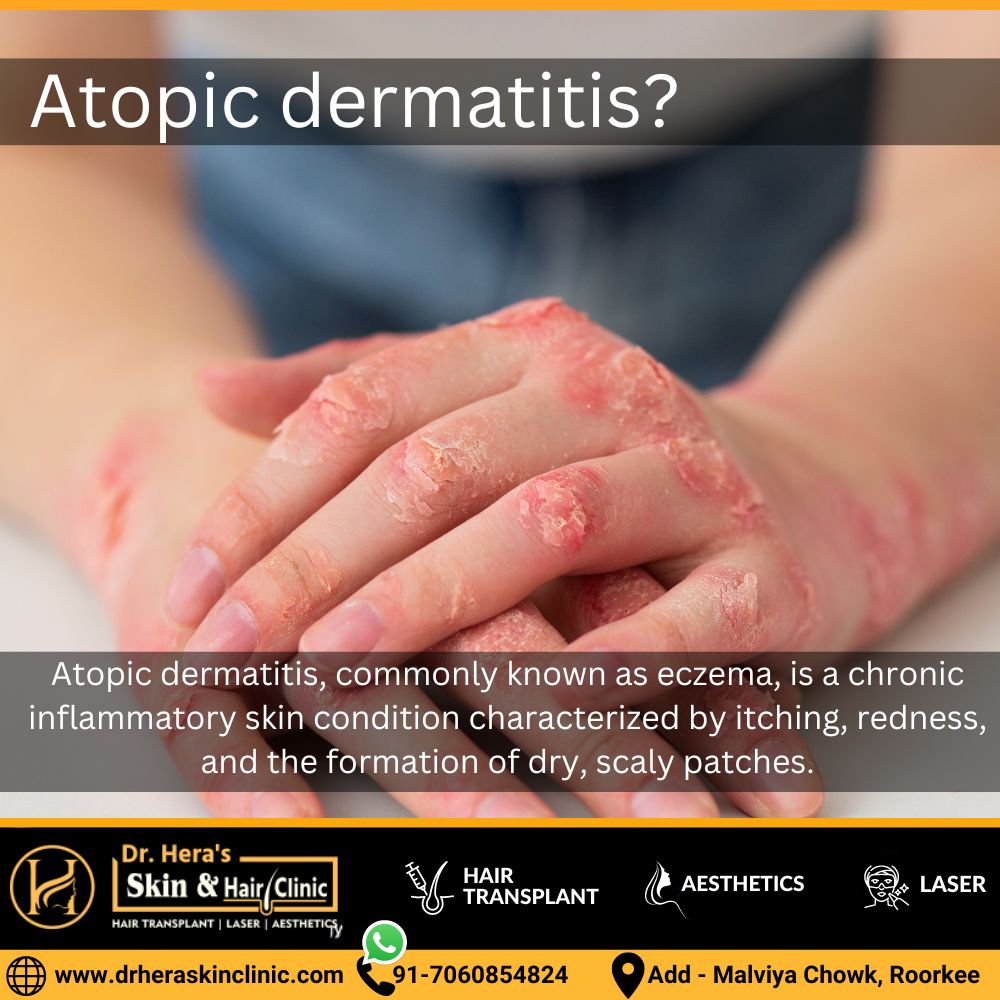
Atopic dermatitis
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition characterized by itching, redness, and the formation of dry, scaly patches. Atopic Dermatitis Treatment strategies aim to alleviate symptoms and improve the skin barrier function. Common approaches include:
Topical Corticosteroids:
These anti-inflammatory creams or ointments help reduce itching and inflammation, but their prolonged use requires monitoring for potential side effects.
Topical Calcineurin Inhibitors:
Tacrolimus and pimecrolimus are non-steroidal creams that suppress immune responses, effectively managing atopic dermatitis symptoms without the side effects associated with long-term corticosteroid use.
Emollients and Moisturizers:
Regular application of fragrance-free moisturizers helps maintain skin hydration and reinforces the skin barrier, reducing the frequency and severity of flare-ups.
Antihistamines:
Oral or topical antihistamines may be recommended to alleviate itching and improve sleep quality, especially during nighttime itching episodes.
Phototherapy (Light Therapy):
Controlled exposure to ultraviolet (UV) light under medical supervision can be beneficial in managing moderate to severe cases of atopic dermatitis.
Individualized treatment plans are crucial, and dermatologists may explore various combinations of these approaches based on the severity and specific characteristics of the condition. Regular communication with healthcare professionals helps ensure an effective, tailored strategy for managing atopic dermatitis.
Cause of atopic dermatitis
Atopic dermatitis, commonly known as eczema, is a multifactorial condition with a complex interplay of genetic, environmental, and immunological factors. While the exact cause remains elusive, effective treatment strategies aim to address the underlying mechanisms contributing to the development of atopic dermatitis. Key factors influencing treatment include:
- Genetic Predisposition: Individuals with a family history of atopic dermatitis, asthma, or allergic rhinitis may be genetically predisposed to the condition. Understanding this genetic link can guide personalized treatment plans.
- Immune System Dysfunction: Atopic dermatitis involves an abnormal immune response, leading to inflammation and skin barrier dysfunction. Treatments often focus on modulating immune responses using topical corticosteroids, calcineurin inhibitors, or systemic immunosuppressants.
- Skin Barrier Impairment: Defects in the skin barrier allow allergens and irritants to penetrate, triggering flare-ups. Emollients and moisturizers help restore and maintain the skin barrier, reducing the frequency and severity of symptoms.
- Allergens and Irritants: Identification and avoidance of specific allergens and irritants are crucial. Dermatologists may recommend allergen testing and lifestyle modifications to minimize exposure to triggers.
- Inflammatory Mediators: Elevated levels of inflammatory mediators, such as histamines, contribute to itching. Antihistamines, either topical or oral, are commonly used to alleviate itching and improve sleep.
- Microbial Factors: Bacterial and viral infections can exacerbate atopic dermatitis. Proper hygiene and, in some cases, antimicrobial treatments may be included in the management plan.
A comprehensive understanding of these factors allows dermatologists to tailor treatment plans, combining various approaches to address the individualized nature of atopic dermatitis and provide effective symptom relief. Regular follow-ups with healthcare professionals help monitor progress and adjust treatment strategies as needed.
Treatment for atopic dermatitis treatments
The treatment for atopic dermatitis (eczema) aims to manage symptoms, reduce inflammation, and improve the skin barrier. While there is no cure, various approaches are employed based on the severity of the condition. Common treatments include:
- Topical Corticosteroids: These anti-inflammatory creams or ointments are effective in reducing redness and itching. Dermatologists prescribe them based on the severity of symptoms, and their usage may be tapered over time to minimize side effects.
- Topical Calcineurin Inhibitors: Tacrolimus and pimecrolimus are non-steroidal creams that suppress immune responses and are particularly useful in sensitive areas like the face and neck. They are suitable for long-term use.
- Emollients and Moisturizers: Regular use of fragrance-free moisturizers helps keep the skin hydrated, preventing dryness and minimizing flare-ups. This is a fundamental aspect of managing atopic dermatitis.
- Antihistamines: Oral or topical antihistamines can alleviate itching and improve sleep quality, especially during nighttime itching episodes.
- Phototherapy (Light Therapy): Controlled exposure to ultraviolet (UV) light, often under medical supervision, can be beneficial for moderate to severe cases of atopic dermatitis.
- Systemic Medications: In cases of severe atopic dermatitis, systemic medications such as oral corticosteroids or immunosuppressants may be prescribed. These are typically reserved for short-term use due to potential side effects.
- Allergen Identification and Avoidance: Identifying and avoiding specific allergens or irritants is essential. Allergen testing can guide lifestyle modifications to minimize exposure to triggers.
- Wet Wrap Therapy: In more severe cases, wet wrap therapy may be recommended, involving the application of wet bandages over moisturized skin to enhance the absorption of topical treatments.
Individualized treatment plans, developed in collaboration with dermatologist, are crucial for managing atopic dermatitis effectively. Regular follow-ups and open communication with healthcare professionals help monitor progress and adjust treatment strategies as needed.
